Electrophysiology Studies (EPS)
Electrophysiology studies (EPS) are tests done to understand the nature of abnormal heart rhythms (arrhythmias).
Electrophysiology studies test the electrical activity of your heart to find where an arrhythmia (abnormal heartbeat) is coming from.
These results can help me to decide the correct treatment for your palpitations which may be medicines, radio-frequency ablation, or implant of a heart rhythm device (Pacemakers, Implantable Defibrillators etc.)
These studies take place in a special room called an electrophysiology (EP) lab or catheterization (cath) lab.
I administer local anaesthetic (injection) at the site of access which is usually a vein in the top of your right leg (groin) area through which I pass electrical cables called catheters to your heart.
Once in position, I can control the electrical activity of your heart and study the pattern to identify any abnormal electrical circuitry as the cause of your symptoms.
Often during these studies, I provoke the electrical system of your heart to reproduce the abnormality that causes palpitations and therefore you may feel that your heart is racing but this is controlled induction of your symptom which I will be able to stop once I have identified the cause of it.
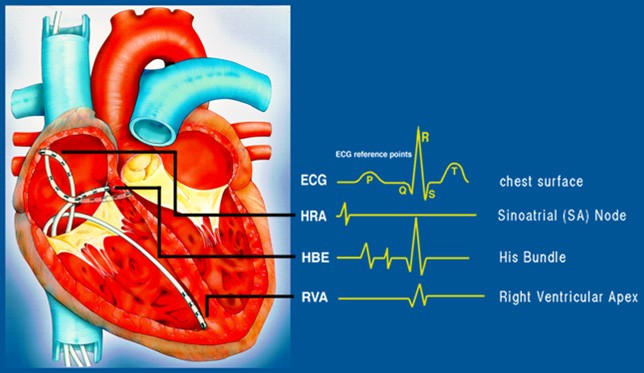
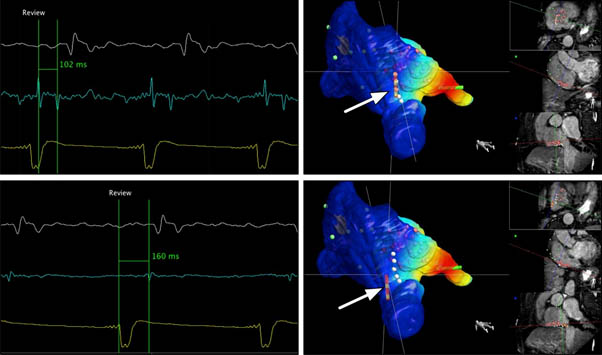
During an EPS, about 3 to 5 electrically sensitive catheters are placed inside the heart to record electrical activity.
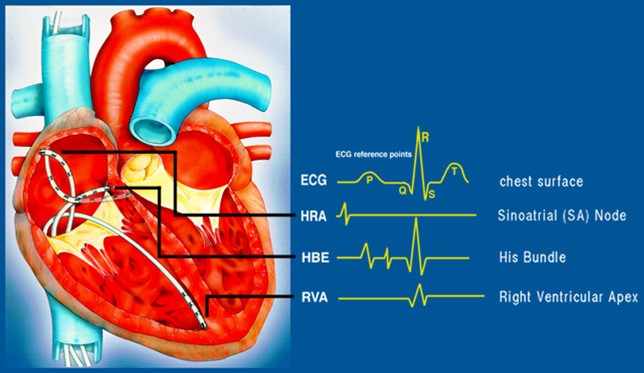
STANDARD DIAGNOSTIC EPS (Catheters in position)
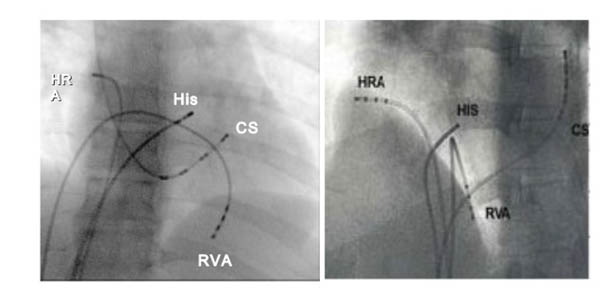
ADVANCED EP STUDIES (3 Dimensional Mapping Studies)
What are the risks of EPS?
A simple diagnostic EP study is potentially free of fatal risks however risks may occur that necessitate specific intervention and includes:
Serious heart rhythm disturbance (Arrhythmias) such as ventricular tachycardia or ventricular fibrillation may occur which may make you dizzy or even lose consciousness. If this happens, I may need to give your heart an electric shock to bring back a regular heartbeat.
Blood clots sometimes can form at the tip of the catheter, break off and block a blood vessel. It is routine to administer a small dose of blood thinning medicine called Heparin to prevent this.
Bleeding, bruising or infection at the site where the catheter went in (groin, arm or neck). I will take every precaution to avoid these problems.
What preparation is needed for EPS?
Don’t eat or drink anything for 6 to 8 hours before the test.
Tell me or anyone in the team about any medicines you take, including over-the-counter medicines, herbs and vitamins.
You will be advised to stop certain medicines that might have been prescribed for control of your palpitations as it is essential to induce the rhythm disturbance on the table to understand the electrical problem.
Have someone to take you to your appointment and take you home.
How long does EPS last?
A simple diagnostic EPS usually last less than an hour, however, if this is associated with radio-frequency ablation to destroy the abnormal electrical connections by a spot welding type technique (as is often the case) it can take even up to 4 hours.
What happens after EPS?
EPS is often followed by a definitive procedure such as Radiofrequency ablation at the same sitting. If you were advised only diagnostic EP studies, then I will discuss results of the test immediately and give you a detailed report along with my recommended treatment.
What will I experience after EPS?
You may feel a bit tired and drowsy from the effects of medications given during the study.
You are likely to stay overnight to ensure no adverse complications have occurred from the procedure but increasingly patients are sent home the same day. If the procedure was done for non-serious heart conditions and you did not have an ablation, it is reasonable to expect to get hioem the same day but you need to be aware to watch for the following
1) The puncture site may be sore for several days.
2) A small bruise at the puncture site is normal. If the site starts to bleed, lie flat and contact me or someone in my team immediately.
Please call the hospital or me directly if you notice any of the following
A sudden increase in swelling around the puncture site.
Bleeding doesn’t slow down when you press hard on the site.
Your arm or leg that was used for the sheath feels numb or tingles.
Your hand or foot feels very cold or changes colour.
The puncture site looks more and more bruised.
The puncture site begins to swell or fluids begin to come from it.